When most people see the word “rabies,” they think of rabid dogs, raccoons, skunks, and foxes. While those are certainly vectors of the viral disease, Bryan Simon, co-owner of Vertical Medicine Resources and Associate Editor for the American Alpine Club’s yearly guide, Accidents in North American Climbing, wants outdoor enthusiasts to think of bats, too.
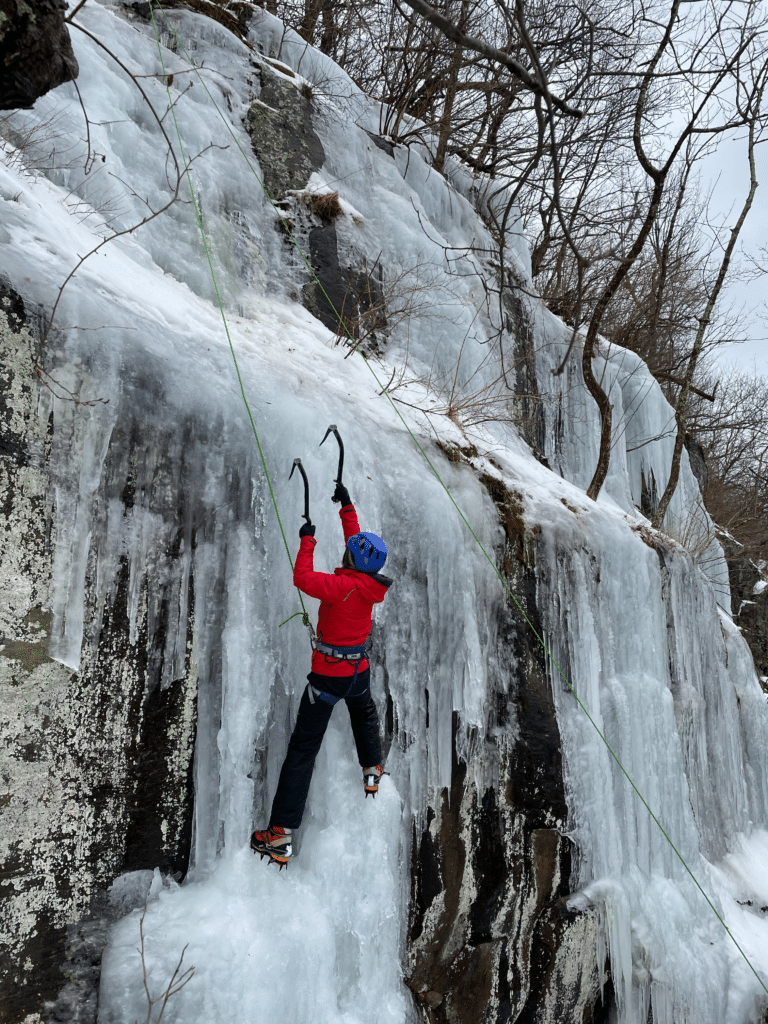
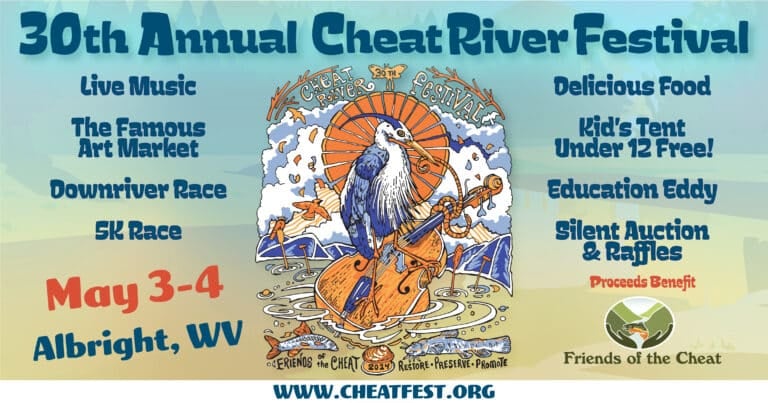
“They’re one of the most common vectors we as outdoor enthusiasts encounter here in the U.S.,” says Simon, who himself was bitten by a bat while climbing in June 2015, just a year after he wrote a report for Accidents in North American Climbing on a climber-bat incident at the Bozoo rocks in West Virginia.
In nearly all instances, rabies left untreated is fatal, which is why it’s so important that patients receive post-exposure prophylaxis and human rabies immune globulin within 24 hours of the animal bite. Even more importantly, the Centers for Disease Control and Prevention recommends that anyone who even suspects having come into contact with a bat should receive the vaccine, just to be safe.
Wake up after a night in an Appalachian Trail shelter and see bats roosting in the rafters? Get the vaccine. Pull your hand out of a crack, see a bat inside, but don’t feel any pain on your hand? Definitely, definitely get the vaccine.
“This is not something to joke around about,” Simon says. “A lot of times people who don’t have a lot of pain, they tend to ignore the injury.”
But when it comes to rabies, playing the “tough guy” card can result in loss of life.
What to do:
- Know signs and symptoms of rabies in animals. This includes foaming at the mouth and erratic or abnormal behavior.
- Be aware of your surroundings. Avoid sleeping in areas where bats are known to roost or where bat guano is clearly present.
- Should you be planning to travel overseas to areas where rabid dogs are common, consider getting a pre-exposure rabies vaccine. “It is fairly expensive,” says Simon, “and if you’ve been bitten by an animal that you suspect has rabies, whether you’ve had the rabies vaccine or not, you still need to get to the hospital as soon as possible.” The difference in the end is two post-exposure doses versus the four you will need (plus the human rabies immune globulin) if you have not had a pre-exposure vaccine.
- If you so much as suspect you have been exposed to bats or other rabid animals, seek medical care immediately. “It’s a medical urgency, not emergency,” Simon adds. “I wouldn’t want someone speeding 80 miles per hour down the interstate, but you need to get out of wherever you’re at and to a hospital within 24 hours.”
- Call nearby hospitals to see which one carries the post-exposure prophylaxis. “Certainly don’t go to an urgent care. They’re not going to have what you need, and some hospitals even don’t carry everything. It pays to call ahead.”
- Wash bite site immediately with soap and copious amounts of water.
- Begin post-exposure prophylaxis within 24 hours of incident. Additional doses must be taken on days 3, 7, and 14 after the first vaccination.
Read more about worst-case scenarios here.